 ICD-10 = Q99.9 or Q93.89
ICD-10 = Q99.9 or Q93.89
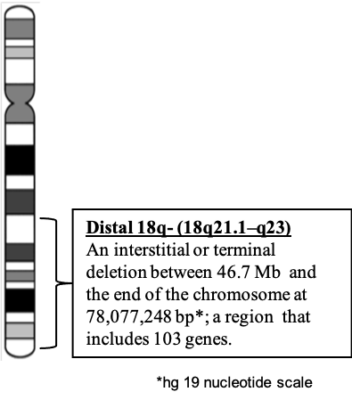
These recommendations are inclusive of the entire population of people with Distal 18q deletions even though each person has a unique deletion. Therefore each person’s deletion could have different genes that are hemizygous. The specific hemizygous genes for an individual patient will dictate the probability of particular phenotypes. Guidance for creating an individualized plan for evaluation and management based on the person’s specific deletion can be found in the next section. However, the information in this document encompasses the global distal 18q- evaluation and management plan.

